Noticeable & Increased Profit
HealthUnits utilizes an advanced analytical system to evaluate practice performance,
identifying flaws and inefficiencies. Our skilled staff has achieved noticeable success
and increased revenue by addressing these issues.
Performance analysis generates extensive reports for clients, offering critical insights and comprehensive assessments of practice performance. These reports enable medical providers to implement effective reforms early, ensuring the continued success of the organization.
Performance analysis generates extensive reports for clients, offering critical insights and comprehensive assessments of practice performance. These reports enable medical providers to implement effective reforms early, ensuring the continued success of the organization.

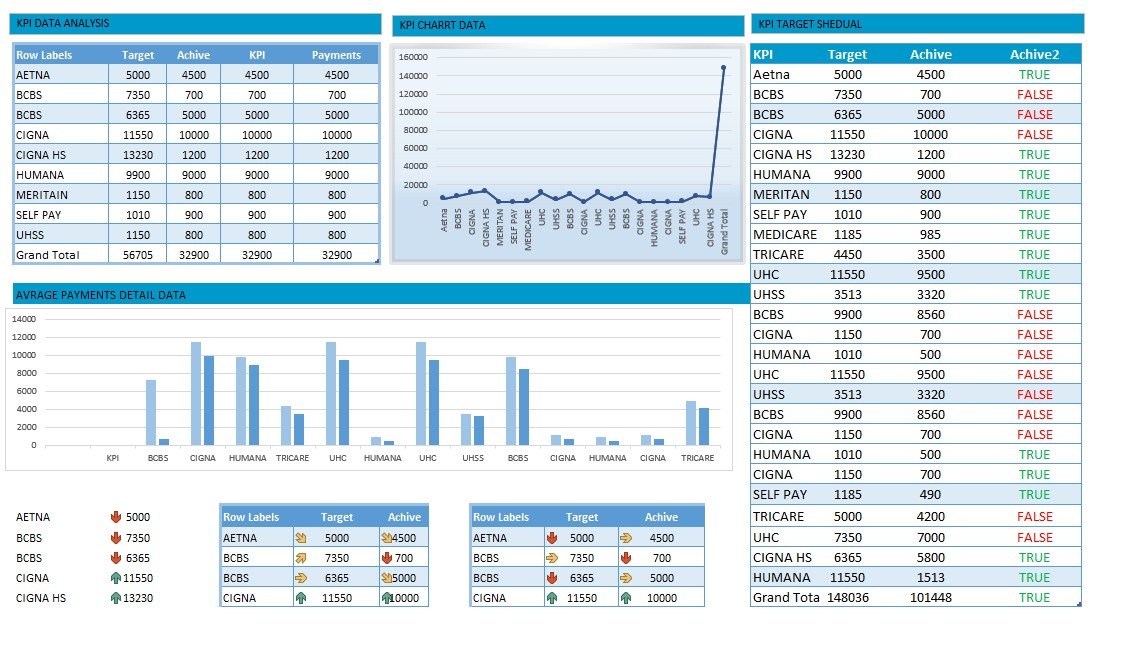
Statistical Analysis of KPIs
Maintaining key performance indicators (KPIs) demonstrates an organization's
commitment to overseeing its entire process. KPIs monitor the average time a claim
takes to be paid, with a benchmark set at 30 to 35 days for accounts receivable. Meeting
this performance metric ensures a healthier practice with smooth cash flow.
The clean claims or first-pass claims ratio significantly impacts practice health, as clean claims process faster than denied ones. We measure the total time spent on claim rework and identify the reasons for denials to avoid delayed processing.
Understanding major payers and their requirements is essential for optimal performance. We continuously monitor annual fee schedules and renew expired contracts with major payers. Adhering to payer requirements ensures that services or codes are covered under the patient’s current plan. Additionally, tasks such as obtaining prior authorization, applying correct modifiers, and accurately capturing patient demographics are crucial for maintaining superior performance.
The clean claims or first-pass claims ratio significantly impacts practice health, as clean claims process faster than denied ones. We measure the total time spent on claim rework and identify the reasons for denials to avoid delayed processing.
Understanding major payers and their requirements is essential for optimal performance. We continuously monitor annual fee schedules and renew expired contracts with major payers. Adhering to payer requirements ensures that services or codes are covered under the patient’s current plan. Additionally, tasks such as obtaining prior authorization, applying correct modifiers, and accurately capturing patient demographics are crucial for maintaining superior performance.
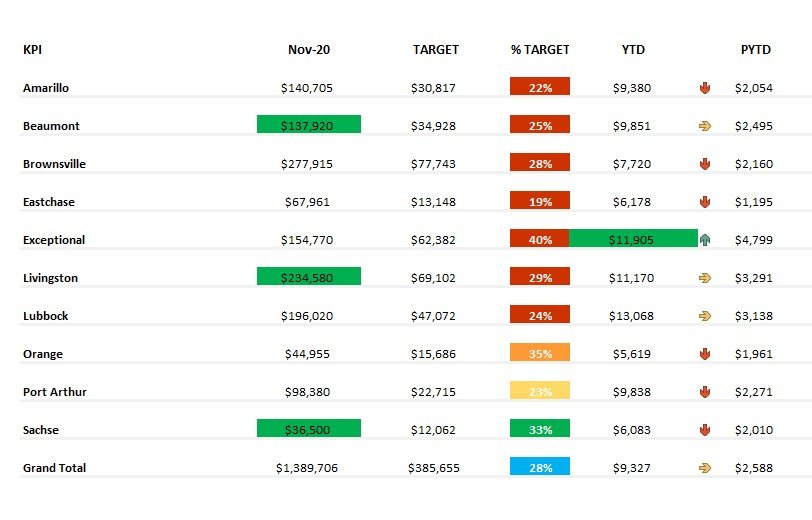
Trustworthy Measures of Quality
Intelligent reports based on clinical services provide a clear vision for estimating an
organization's current statistics. Quality is a cornerstone of any business, and
substandard performance can lead to irregular reimbursements and a decline in practice success.Intelligent reports based on clinical services provide a clear vision for estimating an
organization's current statistics. Quality is a cornerstone of any business, and
substandard performance can lead to irregular reimbursements and a decline in practice success.
HealthUnits employs a modern model of clinical analysis that includes Meaningful Use (MU), Provider Quality Reporting System (PQRS), Pay for Performance (P4P), PatientCentered Medical Home (PCMH), and Accountable Care Organizations (ACOs).
This model showcases both financial and economic analytics. Our technical analysts deliver comprehensive insights into clinical services and the operational performance of the organization, ensuring both quality and efficiency.
HealthUnits employs a modern model of clinical analysis that includes Meaningful Use (MU), Provider Quality Reporting System (PQRS), Pay for Performance (P4P), PatientCentered Medical Home (PCMH), and Accountable Care Organizations (ACOs).
This model showcases both financial and economic analytics. Our technical analysts deliver comprehensive insights into clinical services and the operational performance of the organization, ensuring both quality and efficiency.
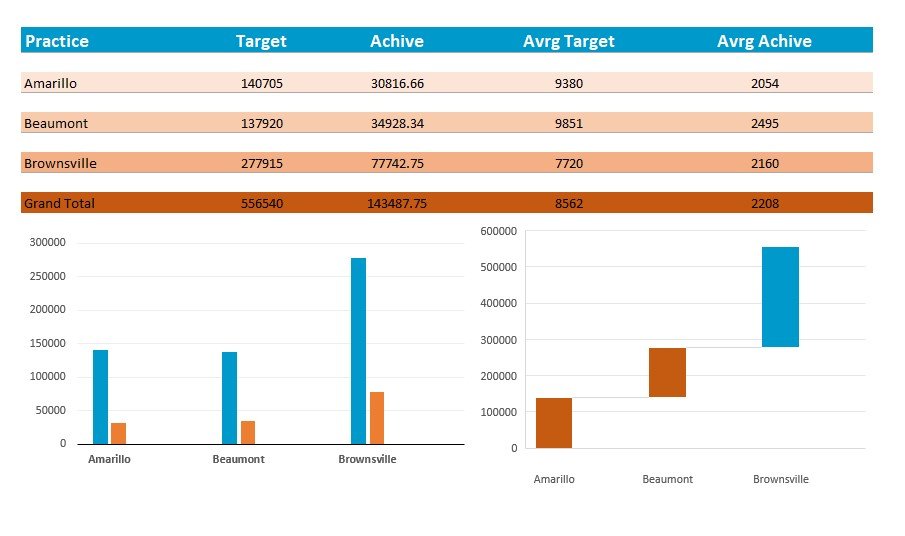
Provider Productivity Metrics
A broad range of reports is compiled to gauge the performance and productivity of
providers. These reports are created through the mutual collaboration of healthcare technical consultants and analysts, with managers organizing the informational data.
The acquired information includes:
- Measurement of individual provider productivity and its impact on the practice.
- Comparison with multiple practices to determine if benchmarks were met, highlighting strengths and weaknesses.
- These reports encourage provider responsibility and promote a high-quality culture by providing a clear view of performance and services.
- Providers are educated on the proper use of evaluation and management codes to prevent revenue loss due to incorrect coding.
- Measurement of individual provider productivity and its impact on the practice.
- Comparison with multiple practices to determine if benchmarks were met, highlighting strengths and weaknesses.
- These reports encourage provider responsibility and promote a high-quality culture by providing a clear view of performance and services.
- Providers are educated on the proper use of evaluation and management codes to prevent revenue loss due to incorrect coding.